Advancing Indigenous Tuberculosis Elimination: Policy, Partnerships, and Community Empowerment
By Madelyn Roy
Introduction
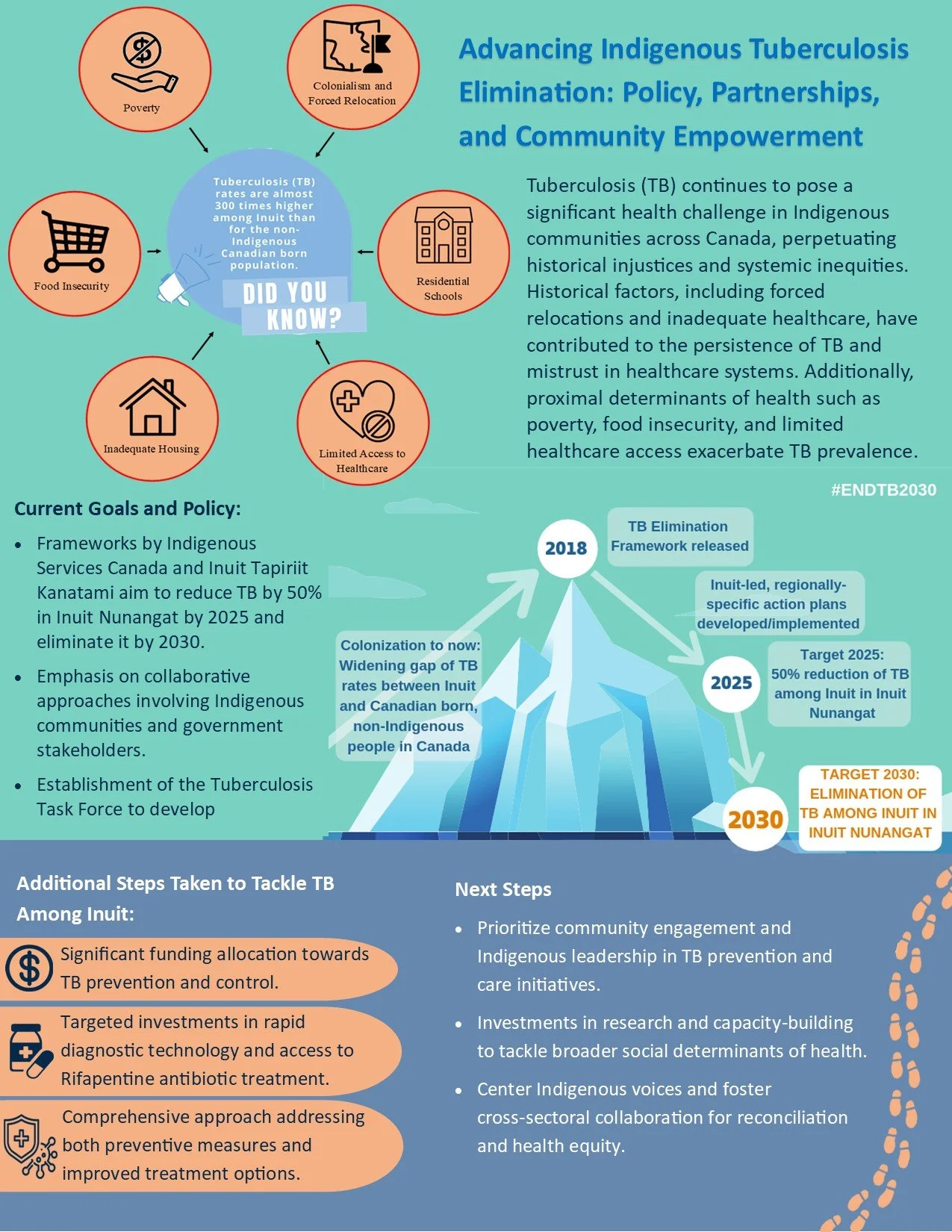
Tuberculosis (TB) remains a pressing health concern within Indigenous communities across Canada, highlighting the urgent need for concerted efforts to address the underlying social inequities driving its prevalence. These communities endure disproportionately high rates of TB, underscoring the enduring legacy of historical and ongoing systemic injustices (PHAC, 2014). To effectively address this challenge, it is imperative to understand the intricate interplay between TB and Indigenous health policy.
The introduction of TB to Indigenous communities in Canada can be traced back to European colonization and subsequent displacement of Indigenous peoples from their ancestral lands. Colonial policies, including forced relocations and inadequate healthcare provision, exacerbated the spread of TB and impeded effective management (Heffernan et al., 2022). Furthermore, the profound consequences of the residential school system continued to propagate the spread of tuberculosis among Indigenous children, perpetuating intergenerational trauma and fostering deep-seated mistrust of the healthcare system (Kim, 2019). Beyond historical factors, TB prevalence within Indigenous communities is influenced by various proximal determinants of health, including poverty, food insecurity, inadequate housing, and limited access to healthcare. Economic disparities and food insecurity amplify TB risk, while overcrowded and poorly ventilated living conditions serve as breeding grounds for transmission (PHAC, 2014; ITK, 2018). Moreover, geographical barriers and cultural insensitivity impede access to healthcare services, underscoring the urgent need for comprehensive, culturally competent interventions (PHAC, 2014; ITK, 2018).
The increased prevalence of tuberculosis (TB) within Indigenous communities in Canada underscores the urgent need for comprehensive policy interventions that address historical injustices and systemic barriers to healthcare access. By recognizing the enduring impact of colonization on Indigenous health outcomes, policymakers can prioritize culturally sensitive approaches that empower Indigenous communities in TB prevention and care initiatives. Additionally, fostering collaboration between government agencies, healthcare providers, and Indigenous leaders is essential for developing and implementing effective policies that promote health equity and reconciliation. Through concerted efforts to address the social determinants of health and center Indigenous voices in policy-making processes, we can work towards achieving tangible progress in TB elimination and advancing Indigenous health and wellness across Canada.
Current Goals and Policy
A comprehensive framework developed by Indigenous Services Canada and Inuit Tapiriit Kanatami outlines efforts to eliminate TB within Indigenous communities. They aim to reduce the incidence of TB in Inuit Nunangat by half by 2025 and complete elimination by 2030 (Indigenous Services Canada, 2018; ITK, 2018). These frameworks recognize the urgent need to address the historical and ongoing disparities in TB burden faced by Indigenous populations and prioritize collaborative approaches involving Indigenous communities, governments, and other stakeholders.
The establishment of the Tuberculosis Task Force in response to the disproportionately high rates of TB among Inuit communities highlights the government's commitment to addressing this pressing health issue (Indigenous and Northern Affairs Canada, 2017). This task force serves as a platform for intersectoral collaboration, bringing together representatives from Indigenous communities, provincial and territorial governments, and other partners to develop and implement a comprehensive strategy for TB elimination across Inuit Nunangat (Indigenous and Northern Affairs Canada, 2017). By leveraging existing processes and engaging with key stakeholders, the task force aims to define the Inuit approach to TB elimination through meaningful community consultation and participation.
Additional Steps Taken by the Government of Canada to Tackle TB Among Inuit
In addition to the establishment of the Tuberculosis Task Force, the Government of Canada has taken several concrete actions to address TB among Inuit communities. These actions reflect a commitment to improving health outcomes and reducing health disparities for Indigenous peoples, particularly in the context of TB prevention and control.
The 2017 federal budget allocated significant funding towards improving the health outcomes of First Nations and Inuit communities, including $13 million specifically earmarked for TB prevention and control, with over $1 million targeted towards Inuit populations (Indigenous and Northern Affairs Canada, 2017). This funding demonstrates the government's recognition of the need for targeted investments to address the unique health challenges faced by Inuit communities, including the high rates of TB incidence.
Furthermore, the Government of Canada has supported initiatives aimed at enhancing TB prevention, diagnosis, and treatment within Inuit Nunangat. Investments in rapid TB diagnostic technology have been made to improve access to early detection and treatment in regions experiencing high rates of TB (Indigenous and Northern Affairs Canada, 2017). The government has facilitated access to Rifapentine, an antibiotic used in TB treatment, to address latent TB infection in areas with high disease prevalence (Indigenous and Northern Affairs Canada, 2017). These efforts reflect a comprehensive approach to TB elimination, encompassing both preventive measures and enhanced treatment options to reduce TB transmission and improve health outcomes for Inuit communities.
Overall, the Government of Canada's actions to address TB among Inuit populations demonstrate a commitment to collaborative, evidence-based approaches to TB prevention and control. By investing in targeted initiatives, engaging with Indigenous communities, and leveraging partnerships with key stakeholders, the government is working towards achieving the goal of TB elimination and improving health equity for Inuit peoples.
Next Steps Needed
While these policy initiatives represent significant progress, there remains a need for further action to fully address the complex challenges surrounding TB within Indigenous communities. Policymakers should prioritize enhancing community engagement and empowering Indigenous leadership in the design and implementation of TB prevention and care initiatives (Gouldhawke, 2021). This includes fostering meaningful partnerships between government agencies, Indigenous organizations, healthcare providers, and community members to ensure that policies and programs are culturally relevant, responsive, and effective (Gabel et al., 2017).
Policymakers should prioritize investments in research, surveillance, and capacity-building initiatives aimed at addressing the broader social determinants of health that contribute to TB prevalence among Indigenous populations (ITK, 2018). By addressing underlying issues such as poverty, food insecurity, inadequate housing, and limited access to healthcare, policymakers can create environments that support TB elimination and promote health equity within Indigenous communities (Gouldhawke, 2021). Additionally, efforts should be made to expand access to culturally competent TB prevention and care services, including the provision of rapid diagnostic technology and innovative treatment options tailored to the unique needs and contexts of Indigenous communities (Indigenous and Northern Affairs Canada, 2017).
In conclusion, while significant strides have been made in advancing Indigenous health policy and practice related to TB elimination, ongoing collaboration, community engagement, and targeted investments are essential to achieving the goal of TB elimination and promoting health equity within Indigenous communities (Gabel et al., 2017; Indigenous and Northern Affairs Canada, 2017). By centering Indigenous voices, fostering cross-sectoral collaboration, and addressing the underlying social determinants of health, policymakers can work towards achieving reconciliation and improving health outcomes for Indigenous populations affected by tuberculosis.
References
Gabel, C. DeMaio, P. & Powell, A. (2017). Towards healthier Indigenous health policies? Navigating the labyrinth for answers. Journal of Indigenous Wellbeing Te Mauri-Pimatisiwin 2(1), p. 47-59.
Gouldhawke, M. (2021). The failure of Federal Indigenous Healthcare Policy in Canada. Yellowhead Institute. https://yellowheadinstitute.org/2021/02/04/the-failure-of-federal-indigenous-healthcare-policy-in-canada/
Heffernan, C., Ferrara, G., & Long, R. (2022). Reflecting on the relationship between residential schools and TB in Canada. The international journal of tuberculosis and lung disease: the official journal of the International Union against Tuberculosis and Lung Disease, 26(9), 811–813. https://doi.org/10.5588/ijtld.22.0371
Indigenous and Northern Affairs Canada (2017). Tuberculosis Task Force. https://www.canada.ca/en/indigenous-northern-affairs/news/2017/10/tuberculosis_taskforce.html
Indigenous Services Canada. (2018). Eliminating Tuberculosis across Inuit Nunangat by 2030; at least a 50% reduction by 2025. From: Indigenous Services Canada. https://www.canada.ca/en/indigenous-services-canada/news/2018/03/eliminating-tuberculosis-across-inuit-nunangat-by-2030-at-least-a-50-reduction-by-2025.html
Inuit Tapiriit Kanatami (ITK). (2018). Inuit tuberculosis elimination framework. https://itk.ca/wp-content/uploads/2018/12/FINAL-ElectronicEN-Inuit-TB-Elimination-Framework.pdf
Kim, P. J. (2019). Social Determinants of health inequities in indigenous Canadians through a life course approach to colonialism and the Residential School System. Health Equity, 3(1), 378–381. https://doi.org/10.1089/heq.2019.0041
P. H. A. C. (2014). Chapter 14: Canadian Tuberculosis Standards 7th Edition: 2014 – Tuberculosis prevention and care in first nations, Inuit and Métis peoples. https://www.canada.ca/en/public-health/services/infectious-diseases/canadian-tuberculosis-standards-7th-edition.html
Madelyn Roy is a medical student with a background in global health, having completed a Master's in Global Health Systems at Western University. With experience in community health research in Uganda, she is passionate about addressing health disparities, particularly in underserved populations. She aspires to work in global health, focusing on improving healthcare systems and reducing health inequalities in underserved communities through both clinical practice and public health initiatives.